Robert M. Kershner, M.D., F.A.C.S .
Clinical Professor, University of Utah School of Medicine, Moran Eye Center,
Salt Lake City, Utah
Ik Ho Visiting Professor of Ophthalmology, Chinese University of Hong Kong
Director Emeritus of Cataract and Refractive Surgery and
Anterior Segment Fellowship Program, Eye Laser Center Tucson, Arizona USA
Consultant Specialist-Ophthalmic Surgical Product and Technology Development
Eye Laser Consulting
Suite 19E
Two Avery Street
Boston, MA 02111-1003
e-mail:
Kershner@EyeLaserConsulting.com
Today's surgeons have access to a complete spectrum of ophthalmic viscosurgical devices (OVDs), previously known as viscoelastics. Ophthalmic viscosurgicals are surgical devices, meaning they can behave and be used as “instruments.” As surgical instruments, OVDs have helped improved cataract surgery to the point where even difficult cases can be managed in a much safer and reproducible manner. These OVDs and other surgical advances have given surgeons more options regarding their surgery including new choices of lenses for improving vision. The following discussion reviews techniques for using hyaluronate and the most recent advances in aspheric optics for improving vision quality with cataract surgery.
Current spectrum of OVDs
The dispersive products such as 2% hydroxypropymethylcellulose (HPMC) and hyaluronate-chondroitin have low-viscosity, water-like characteristics. Higher-viscosity cohesive agents include the original viscoelastic, Healon Æ (sodium hyaluronate1%) (Pfizer, Inc). Healon is a versatile, forgiving OVD that can be used for virtually any aspect of cataract surgery. Due to its easy insertion and removal, Healon is widely used by surgeons for protecting corneal epithelium, creating a deep anterior chamber, improving control, and facilitating capsulorrhexis.
A more viscous version of Healon is also available—Healon GV Æ (sodium hyaluronate 1.4%) (Pfizer, Inc). Due to its greater viscosity, Healon GV provides the distinct advantage of exhibiting greater substance, which can assist surgeons for manipulating tissues. In addition, Healon GV stays in place better than the classic cohesive agent, Healon. Insertion and removal is also easy, which is another important consideration making it virtually interchangeable with original Healon.
Surgeons now also have access to a viscoadaptive , Healon Æ 5 (sodium hyaluronate 2.3%) (Pfizer, Inc). The benefits of a viscoadaptive such as Healon5 is that it changes characteristics depending on how it is used. When injected slowly, Healon5 acts like a dispersive. Alternatively, when injected rapidly, it acts like a cohesive.
Unlike other OVDs, Healon5 is a very tenacious product, likened to “liquid glass” by surgeons. This device requires purposeful insertion and careful removal. Surgeons can use to their advantage that Healon5 does not move after it is inserted. Healon5 allows surgeons to control tissues and to create and maintain space. Due to its high viscosity, surgeons should take care to work around or under the Healon5, but not within it.
Healon5 meets many needs throughout surgery, including improving control during capsulorrhexis, phacoemulsification, and IOL insertion. Special uses of Healon5 include enlarging small pupils, stabilizing the anterior chamber when there is a capsular tear, creating a tamponade posteriorly after a capsule tear, freeing recalcitrant cortex, and controlling nuclear chips.
OVDs in Cataract Surgery
A clinical study by Steve Arshinoff and colleagues examined whether the use of ophthalmic viscosurgical devices with greater viscosity negatively impact intraocular pressure (IOP) after cataract surgery. 1 Their comparison of Healon, Healon GV, and Healon5 (N=99) involved patients undergoing bilateral cataract surgery. Patients were randomized to one of two treatment arms: Healon5 in 1 eye and Healon GV in the other eye; or Healon in 1 eye and Healon GV in the other eye. At 24 hours, lower viscosity OVDs appeared to cause slightly lower mean elevations in IOP in normal patients. However, the results also found that if the OVD is removed then their use is not associated with postoperative IOP spikes above 21 mm Hg. These results underscore the safety of OVDs as well as the importance of removing any type of OVD at the end of surgery.
The following seven tips help maximize the use of OVDs for improved surgical techniques and patient outcomes in cataract surgery:
Tip #1 : To assist with capsulorrhexis, fill the anterior chamber with Healon to deepen and expand the chamber, thereby reducing stress on the zonules. Reducing stress on the anterior surface of the lens will create a concavity rather than a convexity, making it much easier to tear the capsule without complications. Healon remains in the anterior chamber during phacoemulsification to protect the endothelium and provide control in difficult cases.
Tip #2 : Before performing capsulorrhexis, place Healon5 in the center of the lens surface to act as a tamponade to stretch the capsule and relax the zonular apparatus. Be careful not to overfill the anterior chamber. Placing Healon5 onto the center of the capsule before performing capsulorrhexis allows surgeons to use Healon5 as a template to work around as they tear, creating a reproducible capsulorrhexis of 5 to 5.5 mm each time. The bolus of Healon5 at the center creates a slight concavity, thereby allowing surgeons to pinch the capsule adjacent to the Healon5 bolus and conduct the tear in a continuous fashion.
Tip #3 : After placing a small bolus of Healon5 at the start of the capsulorrhexis procedure, apply a small bolus of Healon5 under the incision when exiting with the cannula. This technique will aid insertion and passage of the phaco tip, helping to avoid the iris and endothelium. At the start of phacoemulsification, aspirate the Healon5 to prevent visco-occulsion.
Tip #4 : For controlled IOL implantation, use Healon to enlarge and expand the capsular bag and Healon GV or Healon5 for positioning. This approach is preferable to filling the capsular bag and entire anterior chamber with Healon5, which creates a closed-system that can lead to an unfavorable hydraulic-like condition for IOL injection impeding the release of the IOL.
Tip #5 : After expanding the capsular bag with Healon, place a bolus of Healon5 in the center of the bag and insert the IOL injection cartridge directly underneath the bolus. Release the lens underneath the bolus. Healon5 acts as a second instrument to assist pushing the lens downwards into the bag. This approach helps control the IOL during the implantation procedure and keeps the IOL securely in the bag.
Tip #6 : Due to its high degree of lubricity, which will aid IOL insertion, apply Healon5 directly into the injector cartridge. The lubricity will aid in advancing the IOL into the injector cartridge and for releasing the lens out of the nose cone. In-the-bag insertion becomes a simple, reproducible, one-step procedure.
Tip #7 : It is important to remove any OVD material at the end of surgery. To ensure complete removal, place the irrigation and aspiration (I&A) tip onto the surface of the IOL and gently tilt or lift the edge of the lens. Be sure to visually observe removal of the OVD.
Innovations in IOL design
Since the invention of the IOL by Harold Ridley in 1949, IOL design has undergone tremendous advances. Today we have 3-piece IOLs of foldable material, capsular “C” haptics to fixate the lenses in the capsular bag, and square-edged optics to reduce the incidence of posterior capsule opacification (PCO). One of the most recent advances in IOL design involves the application of wavefront technology to change the IOL optics and improve visual quality.
The positive spherical aberration of the cornea, combined with a conventional spherical IOL results in reduced contrast sensitivity. This phenomenon explains why many patients who achieve 20/20 uncorrected visual acuity after cataract surgery experience a worsening of their contrast perception after lens implantation (eg, patients often report they are unable to read small print in low light). All types of spherical IOLs induce high degree of spherical aberration after implantation due to their overall positive sphericity, which underscores the need and potential benefit of a lens that optically counterbalances the positive spherical aberration of the cornea. Based on a population average of corneal spherical aberration, researchers designed an anterior, modified prolate, aspheric IOL (Tecnis Z-9000, Pfizer, Inc.), which replicates the negative spherical aberration of the youthful crystalline lens. This revolutionary new optic design has been tested in numerous trials worldwide and has consistently demonstrated improved visual quality compared to conventional spherical IOLs.
A prospective randomized study compared the effects of an anterior, modified prolate, aspheric IOL with those of a conventional silicone lens (AA4207VF, Staar Surgical) and a conventional acrylic lens (AcrySof Æ SA60AT, Alcon Surgical) on visual performance. 2 The goal of the study was to determine whether the addition of an aspheric optic improves retinal imaging and functional visual performance. Patients (221 eyes of 156 patients) were randomized to receive one of the three IOLs. Test methods included Snellen visual acuity, retinal imaging, functional visual acuity, and contrast testing.
Results indicate that all three IOLs improved visual acuity after cataract surgery (with an average improvement of 20/35 or better). However, patients with the modified prolate lens surprisingly had better visual acuity compared to the other lenses for the first month after surgery. Since the three treatment groups had similar pre- and post-operative refractive errors, the difference in Snellen visual acuity may be due to improved contrast sensitivity with the TECNIS lens.
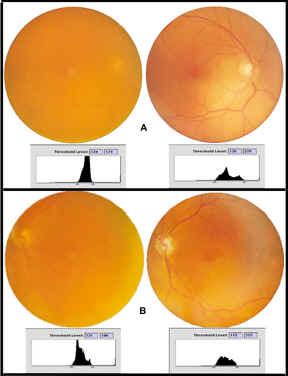
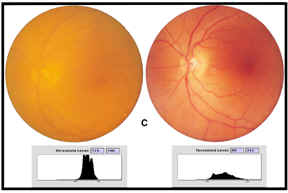
Unlike the conventional spherical lenses, the aspheric lens significantly improved visual performance measured by visual acuity and functional acuity contrast testing. In fact, both types of conventional lenses showed no statistically significant increase in contrast sensitivity during photopic conditions—suggesting that eyes with the aspheric lens saw better even in bright light. Improvements in contrast sensitivity under mesopic conditions were also dramatic, with the TECNIS lens group improving up to 100% (Figure 1). This study also measured retinal image contrast using digital analysis of fundus photography (taken pre- and post-operatively). A comparison of threshold luminance (ie, range of detected contrast of the digital image of the fundus) shows that the contrast levels through the aspheric lens was 28%, which represents a four-fold improvement in contrast (Figure 2).
Summary
Today's full spectrum of OVDs makes surgery more reproducible and safer than ever before. It allows surgeons to tackle more challenging and difficult cases with better outcomes and success. These studies demonstrate that aspheric optics provides better functional visual performance, improved contrast perception especially at night and at night with glare and the best visual improvement overall. The use of the new OVDs combined with the latest advances in high tech aspheric optics, such as TECNIS represent a new generation of IOL technology for improved surgical outcomes and visual performance for today's cataract patients.
References for OVDs and High-Tech IOLs: 7 Secrets to Success
Arshinoff ST, Albiani DA, Taylor-Laporte J. Intraocular pressure after bilateral cataract surgery using Healon, Healon5, and Healon GV. J Cataract Refract. Surg . 2002;28:617-625.
• Kershner RM. Retinal image contrast and functional visual performance with aspheric, silicone, and acrylic intraocular lenses. J Cataract Refract Surg . 2003;29:1684-1694.
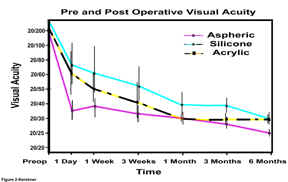
Kershner-Preoperative best-corrected and postoperative uncorrected visual acuity at six months for each of the IOL groups

Kershner-A)
Comparison of aspheric, silicone, acrylic IOLs and preoperative cataract
on Functional Acuity Contrast Testing (F.A.C.T.) of day vision (Photopic)
B)
Comparison of aspheric, silicone and acrylic IOLs on Functional Acuity
Contrast Testing (F.A.C.T.) of day vision with glare
C)
Comparison of aspheric, silicone, acrylic IOLs and preoperative cataract
on Functional Acuity Contrast Testing (F.A.C.T.) of night vision (Mesopic)
D)
Comparison of aspheric, silicone, acrylic IOLs and preoperative cataract
on Functional Acuity Contrast Testing (F.A.C.T.) of night vision with
glare
Kershner
A)
Fundus photography of preoperative cataract (left image) and postoperative
silicone IOL (right image) at 3 months with threshold luminance maps
B)
Fundus photography of Preoperative Cataract (left image) and postoperative
acrylic IOL (right image) at 3 months with threshold luminance maps
C)
Fundus photography of preoperative cataract (left image) and postoperative
aspheric IOL (right image) at 3 months with threshold luminance maps
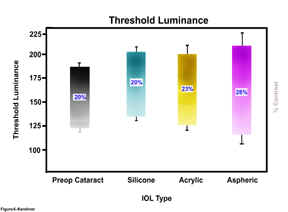
Kershner-Threshold
Luminance Ranges for preoperative cataract, silicone, acrylic and aspheric
IOLs (with percent contrast for each group)
©2004. Robert M. Kershner, M.D., F.A.C.S. All rights reserved.
Robert M. Kershner, MD, FACS-Eye Laser Consulting
e-mail: Kershner@EyeLaserCenter.com
For more
information, visit: http://www.EyeLaserCenter.com/PhysicianResource.htm