Robert
M. Kershner, M.D., F.A.C.S.
Eye
Laser Center
Suite
303, 1925 West Orange Grove Road
Tucson,
Arizona 85704-1152 USA
Phone:
(520) 797-2020 Fax:
(520) 797-2235
©2002. Robert M. Kershner, M.D., F.A.C.S.
Cataract,
IOL and Refractive Surgery, April 28-May 2, 2001,
San Diego, California. The
Perfect Pupil™ was designed and developed by John Milverton, MD of Sydney,
Australia and is manufactured and distributed by Becton Dickinson Ophthalmic
Surgical, Waltham, Massachusetts, USA. Perfect
Pupil™ is a registered trademark of Milvella Pty Ltd. Dr. Kershner is the
director of the Eye Laser Center in Tucson, Clinical Professor of Ophthalmology
at the Moran Eye Center, University of Utah School of Medicine, Salt Lake City,
Utah, and the IK HO Visiting Professor of Ophthalmology at the Chinese
University in Hong Kong. He has authored hundreds of articles on eye
microsurgical techniques and instruments and lectures to ophthalmic surgeons
worldwide. Dr. Kershner has no
proprietary or financial interest in the techniques or instruments described in
this article.
The increased acceptance of topical anesthesia,
phacoemulsification and small, foldable intraocular lenses (IOLs), have made
possible the techniques of clear corneal cataract surgery (1).
Operating through these small (less than 3.0 mm), corneal incisions have
placed new demands on surgeons to effectively and safely remove the cataract and
implant the IOL without increasing the risk of corneal, iris or capsular damage.
Many patients who present for cataract removal have eyes complicated by
pupils with iris sphincter sclerosis due to aging, synechiae, previous trauma or
surgery, diabetes, iridoschisis, uveitis, chronic miotic therapy,
pseudoexfoliation, or chronic lues. The
small pupil (less than 3.0mm) can impede visualization and make instrumentation
into the eye more difficult. Capsulorrhexis can be all but impossible through a
small pupil. Hydrodissection and
phacoemulsification of the lens nucleus can lead to an increased risk of iris
sphincter tear, bleeding, iris emulsification, ruptured posterior capsule and
loss of the nucleus. The postoperative result of these encounters can be an
irregular and atonic pupil, photophobia and discomfort for the patient.
Present methods of dealing with a small pupil at the time of cataract surgery have all had limitations. Pharmacological therapy with the use of non-steroidal eye drops, or strong mydriatics such as 10% phenylephrine, are often associated with untoward ocular and systemic side effects and may be ineffective in dilating bound-down and scarred pupils. The surgeon can simply ignore pupil size and perform the maneuvers of small incision surgery through an unenlarged incision, but this may result in the inadvertent complications described. Many surgeons have turned to mechanical methods and devices to enlarge the pupil at cataract surgery. These include using a blade, needle or scissors to make multiple iris sphincter tears, iris hooks to retract the iris tissue through four or more corneal stab incisions (2), or introducing mechanical stretching devices to pull on the sphincter margin. All of these methods are cumbersome, require specialized instruments, difficult intraocular maneuvers, and are associated with bleeding, permanent loss of iris sphincter function, and abnormal pupil shape postoperatively.
This study was undertaken to assess the protective effect and dilating potential of a new, disposable device for small pupil cataract surgery. Developed by John Milverton, MD of Sydney, Australia, this device was aptly named the Perfect Pupil™. It is a sterile, disposable, polyurethane ring with an integrated arm that allows for easy insertion into the eye and removal at the conclusion of surgery. The device is inserted through an unenlarged clear corneal incision, with the arm remaining outside the eye to aid in easy removal. The procedures of capsulorrhexis, hydrodissection, phacoemulsification and IOL insertion are carried out with the device in place. The Perfect Pupil is then removed at the end of the surgery by reversing the steps used for insertion.
Preoperatively,
the patients received one drop each of topical 1% tropicamide and 2.5%
phenylephrine every five minutes for fifteen minutes prior to surgery. They were
transported to the operating room where a drop of 4% topical povidone iodine was
instilled and surgical prep performed. The patient's eye was draped with a sterile adhesive
disposable drape (Kershner Cataract Drape II- Kimberly Clark Corporation) and
the Kershner reversible eyelid speculum (Rhein Medical, Tampa, Florida USA) was
inserted. All procedures were
performed under topical anesthesia (3). Several
drops of 0.5% tetracaine hydrochloride were instilled.
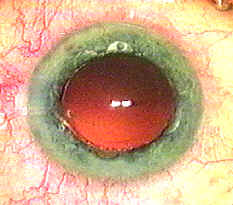
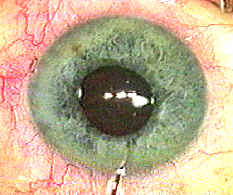
The pupil, as seen through the cornea, was measured through the ocular of
the operating microscope and compared to a known standard pupil gauge chart in
millimeters (mm).
A 2.8 mm clear
corneal incision was created with either a diamond keratome or the BD disposable
clear cornea incision system (Becton Dickinson Ophthalmic Surgical, Waltham,
Massachusetts, USA). Astigmatism
was corrected with an arcuate keratotomy incision (1, 4) or a toric intraocular
lens (IOL). Intracameral sodium
hyaluronate (Healon, Pharmacia, Peapack, New Jersey, USA) was injected into the
anterior chamber.
The
Perfect Pupil™ (figure 1) is a sterile, disposable polyurethane ring with an
internal diameter of 7.0 mm. The ring is open for 45 degrees to allow for the
passage of instruments. There is
one 1.6m tab at the top of the device and five 4mm fenestrations in the ring for
positioning. The iris is firmly
held for 315 degrees by an integrated 0.24 mm flanged groove throughout the
length of the ring. The material is
biocompatible and flexible allowing it to be passed easily through an unenlarged
corneal incision. Once in place,
the device automatically expands the pupil aperture to 7 to 8 mm.
It can be left in place throughout the procedure. The integral arm can be
kept to the side of the corneal incision as a buttress to protect the incision,
keep the device in place within the pupillary space, and to aid in removal at
the conclusion of the surgical procedure. As the ring captures the entire iris sphincter, it acts not
only to dilate the pupil, but it provides unparalleled protection of the iris
sphincter margin avoiding the complications of iris tearing, bleeding,
inadvertent sphincter damage or emulsification.
The
Perfect Pupil is removed from it's sterile tray with forceps (figure 2a-step 1)
and delivered to the incision. The
distal end is coated with a minimal amount of hyaluronate viscoelastic.
The leading edge is then dialed counterclockwise into the anterior
chamber (figure 2b-step 2). A
Sinsky style hook is introduced either through the corneal incision or through a
sideport incision and used to engage the superior tab (step 3).
The iris is engaged and the positioning holes are each used in turn until
the entire pupil is captured inside the flange of the device (step 4).
The pupil size is then remeasured.
Capsulorrhexis
is performed with the Kershner One-Step capsulorrhexis cystotome/forceps (5) or
microcapsulorrhexor (Rhein Medical, Tampa, Florida USA).
Hydrodissection is performed with a Binkhorst cannula and balanced salt
solution by injecting a fluid wave from beneath the sub-incisional cortex to the
opposite side of the capsule until a complete wave is created loosening the
cortical attachments of the lens to the capsule.
Phacoemulsification is performed using a single-instrument,
single-incision technique (6), with a 30 degree tip, 20% phaco power, vacuum
level at 100 mm, and aspiration rate at 20 cc/minute with the Bausch and Lomb
Millennium phacoemulsification machine (Bausch and Lomb, Rochester, New York,
USA). Irrigation and aspiration
(I&A) of residual cortex is completed with the clear cornea I&A tip (Rhein
Medical, Tampa, Florida USA). The
capsular bag is reinflated partially with viscoelastic and the one-piece
Collamer IOL or silicone toric IOL (Staar Surgical, Monrovia, California USA) is
loaded into the microinjection cartridge and inserted into the capsular bag and
centered in one motion.
The
residual viscoelastic is removed with gentle I&A.
The Perfect Pupil is then engaged at the tab with a hook and the pupil
released. The device is backed out
of the incision in the reverse procedure of the insertion by grasping the arm
with a forceps and gently dialing clockwise until removed (step 5).
The pupil is then measured. Subtenons
injection of 0.1 cc of cefazolin (Ancef, Smith Kline Beecham Pharmaceuticals)
and dexamethasone (Celestone, Schering Corporation), is injected and the patient
is discharged for examination the following day.
The
ease of removal of the device from it's tray, insertion of the device into the
eye, and removal of the device at the end of the procedure, as determined by the
surgeon, was similar to insertion of an intraocular lens.
No special instrumentation or surgical techniques were required.
All devices functioned as expected and there were no defects noted in the
manufacture or packaging of the devices used in the study.
The patients, all of whom underwent the procedures under topical anesthesia, were comfortable during the insertion and removal of the device. There were no reported adverse effects experienced by the patients with the use of the Perfect Pupil.
Today's
advanced cataract procedure is more dependent than ever on the successful
execution of a meticulous series of steps from incision construction to
intraocular lens implantation. Adequate
pupillary dilation prior to attempting surgical removal of the cataract is of
critical importance. Many patients
who present for cataract removal have eyes complicated by pupils that do not
adequately dilate despite several pharmacological attempts with topical
mydriatic agents. The causes of
pupils that fail to dilate are numerous, but include iris sphincter sclerosis
due to aging, synechiae, previous trauma or surgery, diabetes, chronic lues,
iridoschisis, uveitis, chronic miotic therapy, or pseudoexfoliation.
When a surgeon encounters a small pupil at the time of cataract surgery,
he or she is left with a decision whether to proceed with the surgery or to
intervene with a procedure that will most probably effect the successful
outcome. In some instances, simply leaving the pupil alone, will suffice.
However, attempting the various steps of cataract surgery through an
undilated pupil can be a challenging and daunting task.
Visualization of the cataract can be impeded by a small pupil.
This can make it difficult to see the lens capsule for a proper
capsulorrhexis. Even if
capsulorrhexis can be performed, attempting to phacoemulsify a cataract through
an undilated pupil can result in iris sphincter tear and emulsification,
bleeding, ruptured capsule, lost nucleus and breach of the vitreous cavity.
Accordingly,
most surgeons will attempt to mechanically dilate the pupil at the time of
cataract surgery if pharmacological agents fail to enlarge the pupil by
themselves. There have been
numerous techniques and instruments utilized for this task.
I classify pupil dilation methods into three types. The first is the mechanical
stretching method. The second
is the cutting method.
The third is the iris retainer method.
In
the first method, the iris is mechanically stretched.
The instruments of choice to perform this can be a pair of hooks
introduced through two stab incisions in the cornea.
The hooks engage the iris sphincter and are pulled in opposite
directions. This results in one or
more tears of the sphincter, which leads to an enlargement of the pupil
aperture. The advantages of this
procedure is that it is simple, and requires no special instruments. The disadvantage is that the iris sphincter is permanently
damaged and the tear cannot be controlled, resulting in bleeding, pigment
dispersion, and an abnormal and non-functional pupil postoperatively.
In
the second method, sharp instruments are used to cut the iris sphincter. The instruments of choice can be a bent needle or intraocular
scissors. The cutting method is
more controlled but requires the use of a large instrument in the eye that can
result in corneal endothelial damage. The
advantages of the method are that the purposeful tears can be made small and
controlled with less effect on the appearance and function of the pupil.
The disadvantages are the same as the stretching method.
The
third method is the iris retainer method. There
have been several devices fabricated for holding the pupil in the enlarged state
(7). The effect of these devices is
to stretch the pupil around a ring and allow the ring to keep the pupil dilated.
The advantages are these devices are sterile, and hold the pupil in the
enlarged state. The disadvantages
with these iris retainers are they are fixed, rigid and difficult to insert into
the eye through a small incision, cumbersome to manipulate when engaging the
sphincter, and they interfere with the instrumentation needed to enter the eye
for the cataract procedure.
The
instrument that does not share these disadvantages with existing pupil dilating
methods, is the Perfect Pupil™. This
device is sterile, disposable, flexible and can be easily inserted through the
smallest of incisions (less than 100 microns).
Because of it’s unique design, the device captures the pupillary
margin, protects the sphincter, does not cause tears or stretching of the iris,
bleeding or pigment dispersion. Because
of the open ring design of the Perfect Pupil™, there is no interference with
instrumentation of the eye. The
device can be left in place for the entire procedure and following completion of
the surgery, the device is just as easy to remove as it is to insert.
I
am not aware of a single study that demonstrates the advantages of a pupillary
dilation method that also affords the protection of the iris that this device is
capable of offering. Indeed, one of
the distinct benefits of the Perfect Pupil™ is it’s ability to fully protect
the pupil it expands. In fact, this
device not only is of benefit to the cataract surgeon encountering a small,
undilated pupil, but could be of benefit to posterior segment surgeons who must
often view the retina and vitreous cavity through small, bound down pupils
during surgery.
The
results of this study demonstrate that when small pupils are encountered (less
than 4.0 mm) the Perfect Pupil™ effectively and consistently dilates the pupil
to almost 8.0 mm. When removed, the
pupil quickly returns to a size approximating the preoperative state (4.3mm).
The resulting surgery leaves the patient with an iris that is
indistinguishable from the appearance prior to surgery, and does not affect the
iris function postoperatively.
A
method that adequately dilates the pupil, prevents iris sphincter damage,
protects the pupil margin, and is easily performed would have decided advantages
for the clear corneal cataract surgeon. The
Perfect Pupil™ is just this superior device, and an excellent addition to
small incision cataract surgery. When encountering pupils that do not adequately
dilate, the surgeon will find the Perfect Pupil™ on the shelf, ready to use,
and easy to insert and remove. The
Perfect Pupil™ expands the pupil to 8mm, protects the iris sphincter during
surgery, and allows the pupil to return to normal size, shape and function
following the clear cornea cataract procedure. It is an excellent adjunct in the
armamentarium of every clear cornea cataract surgeon.
References:
1.
Kershner, RM. Clear corneal
cataract surgery and the correction of myopia, hyperopia and astigmatism.
Ophthalmology 1997;104(3):381-389
2.
Smith GT, Liu CSC. Flexible iris hooks for phacoemulsification in
patients with iridoschisis. J Cataract Refract Surg 2000; 26:1277-1280
3.
Kershner RM. Topical
anesthesia for small incision self-sealing cataract surgery - a prospective
study of the first 100 patients. J
Cataract Refract Surg1993; 19(3):290-292
4.
Kershner RM. Keratolenticuloplasty
- arcuate keratotomy for cataract surgery and astigmatism. J Cataract Refract Surg 1995;21(3):274-277
5.
Kershner RM. A new one-step
forceps for capsulorrhexis. J
Cataract Refract Surg 1990; 16:762-765
6.
Kershner RM. Sutureless
one-handed intercapsular phacoemulsification - the keyhole technique.
J Cataract Refract Surg 1991;
17(Supp):719-725
7.
Graether JM. Graether pupil expander for managing the small pupil during
surgery. J Cataract Refract Surg 1996;22:530-535
Graphics:

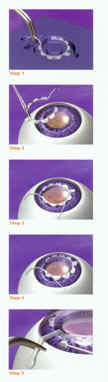
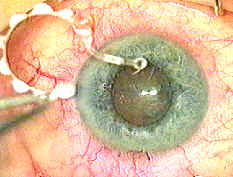
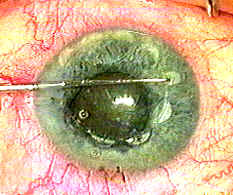
Figure 2a.
Kershner-Step 1-The device is removed from the sterile tray with forceps.
Figure 2b-Kershner
Step 2-Insert Perfect Pupil™ through the clear corneal incision.
Step 3-Use a hook in the positioning holes to engage the pupil edge.
Step 4-Capture the entire pupil into the groove of the ring.
Step 5-Remove Perfect Pupil™ by disengaging the ring with a hook, grasp the arm and withdraw the device through the incision.